Gynaecology
.jpg)
6 Signs Your Daughter is About to Start Her Period
November 12, 2025Puberty comes with many changes for young girls, and one of the most important is menarche, the f...

Menstrual Hygiene: Your Guide to Sustainable, Zero Waste Periods
November 12, 2025Menstrual hygiene remai...

Obesity and Pregnancy: Understanding Weight Gain
November 11, 2025Pregnancy is a life-changing experience, but it can bring additional health considerations for in...

Preparing Together: A Dad's Handbook for Pregnancy
June 16, 2024Becoming a father for the first time is an amazing journey, though it ...

What Is Difference Between PCOD vs PCOS?
April 30, 2024Are PCOD and PCOS the same? A lot of women get confused between the ...

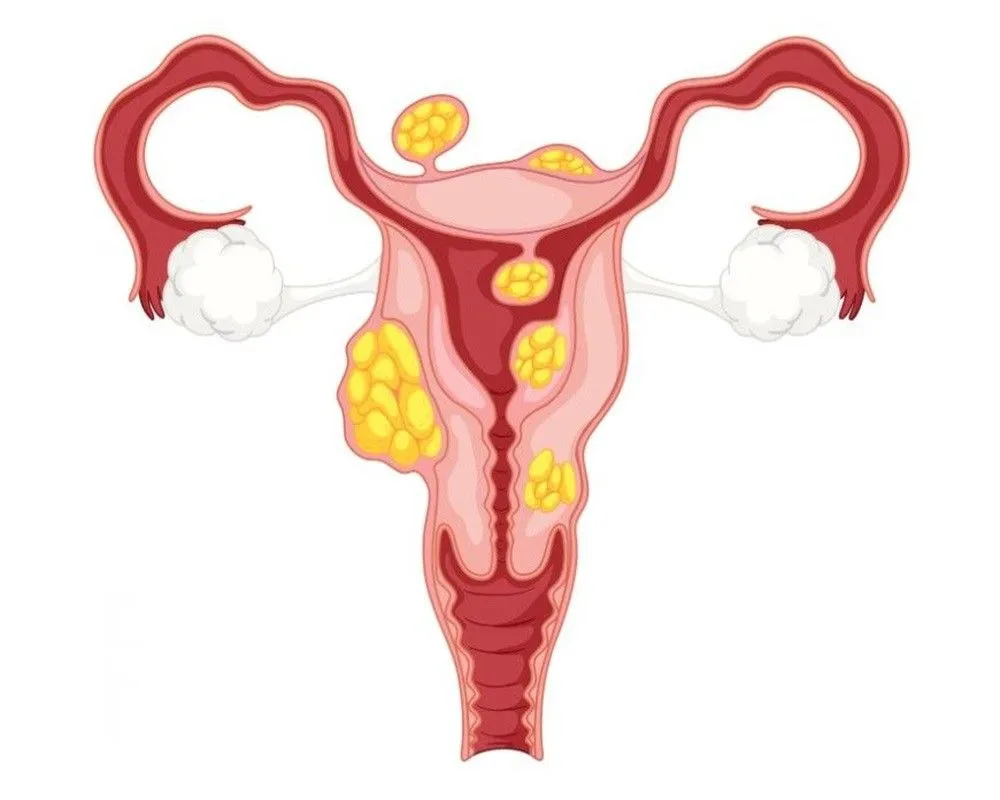
Endometriosis Treatment & Surgery
April 29, 2024What is Endometriosis Endometriosis is a gynaecological condi...

Suction and Evacuation: Procedure, Uses, and Benefits
April 29, 2024Suction and Evacuation is a surgical proc...
Breast Cancer Symptoms & Treatment
April 26, 2024Breast cancer- Be watchful The most commonly heard type ...

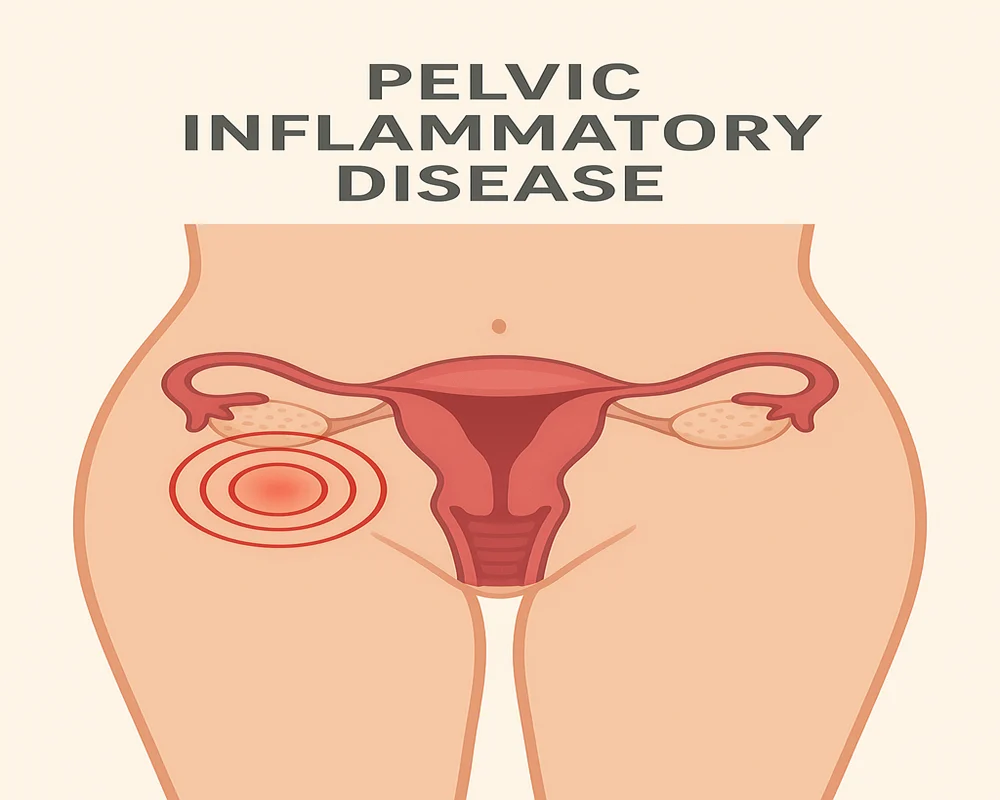
Annual Gynaecology Screening And Its Importance
April 11, 2024Who is a gynaecologist? A gynaecologist is a doctor who ...

Everything You Need To Know About Using Menstrual Cups
March 28, 2024What are menstrual cups? Menstrual cups are product for ...

Considering Minimally Invasive Gynecologic Surgery?
March 26, 2024Minimally Invasive Gynecologic Surgery (MIGS) has come a long way si...

Do Contraceptive Pills Adversely Impact A Woman’s Health?
March 22, 2024Contraceptive pills commonly known as birth control pills or the pil...