Fertility
Different Stages Of An IVF Treatment
April 29, 2024In-vitro Fertilization (IVF) is an effective method to conceive a ch...

6 Ways to Boost Female Fertility
April 22, 2024Each moment awaiting the result of a pregnancy test can feel like ho...

Comparison of A New 3D Automated Volume Calculation Technique (SONO AVC)
April 12, 2024Comparision Of A New 3D Automated Volume Calculation Technique (SONO...

Common Causes of Infertility In Women
April 4, 2024Infertility can be defined as a medical condition that is characteri...
Myths and Facts about Infertility
March 20, 2024Infertility is a complex and often misunderstood condition t...

What Is Infertility
March 14, 2024Infertility is the inability to get pregnant after trying over for a...

Low Estrogen Levels: Causes, Symptoms, and Natural Ways to Boost Them
March 22, 2023Estrogen, often referred to as the “female hormone,” is ...
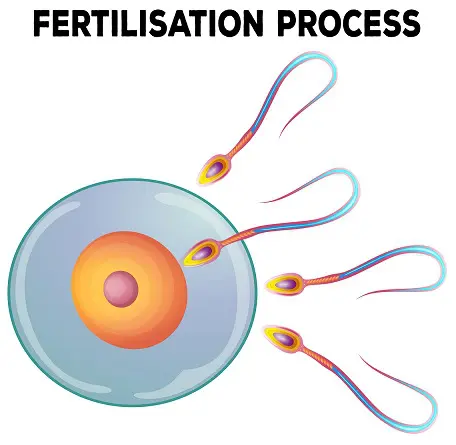
Understanding the Process of Fertilisation
September 30, 2018Understanding the existence of any form...
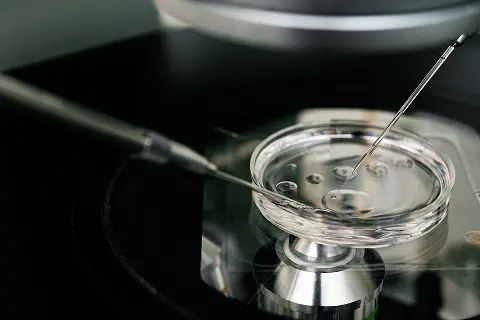
Intracytoplasmic Sperm Injection (ICSI)
September 24, 2018Intracytoplasmic Sperm Injection is a pro...

How to Track Fertility Cycle
December 22, 2016Fertility cycle or menstrual cycle is defined as the changes that oc...

Knowing the Right Time-Fertile Window
December 22, 2016Fertile window refers to the period during which a woman c...

What Causes Infertility in Male & Female
October 7, 2016Infertility is not always a woman’s problem there is also infe...

7 Tips on How to Increase Fertility for Men
August 30, 2016It takes two to create a baby. If your sperm is not strong or health...

4 Keys to preventing infertility in men
August 30, 2016The inability of couples to conceive or become pregnant is a problem...
6 Myths about fertility
August 30, 2016The continuation of life is a natural instinct for any organism. Thi...





