Child Care

Six-Pocket Syndrome and Its Impact on Young People
November 12, 2025Many children grow up in homes where love and attention are abundant. Parents and grandparents pr...

5 Tips to Care for Premature Baby At Home
October 4, 2022Babies born before 37 weeks are known as preterm or premature babies...

Parenting Tips for the First Two Years of Life
September 12, 2022The first year of being a parent can never be easy, no matter how pr...

Impact of Online Education on Kids’ Health
August 8, 2022Ever since the outbreak of the Covid-19 pandemic, our lives have upe...

Monkey pox and its impact on Children & Pregnant Moms
August 5, 2022Everyone has been reading or hearing abou...

Childhood Obesity: Causes, Prevention, and Management of Obesity in Children
March 17, 2022Many children face challenges with healthy weight management. A repo...
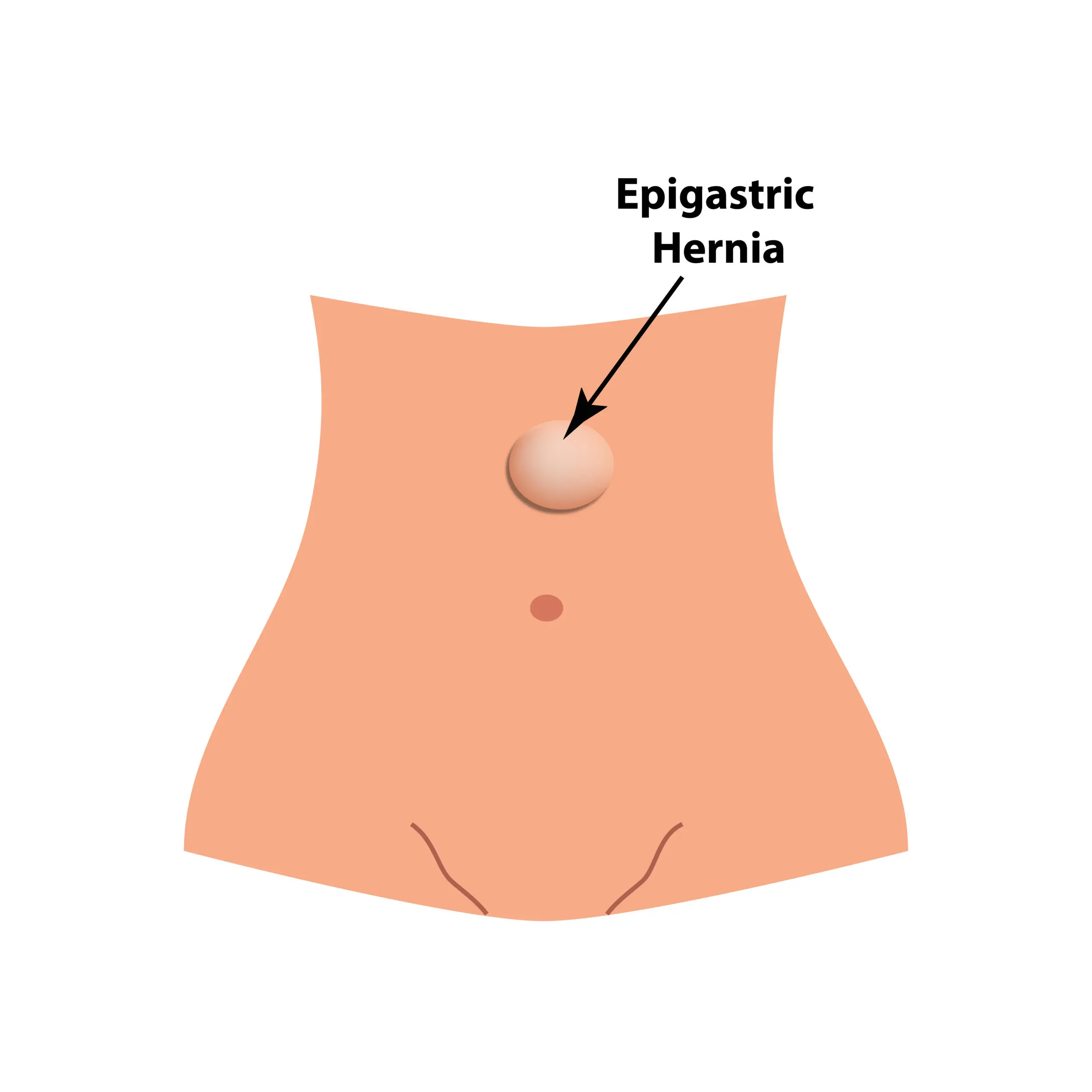
Symptoms & Coping Strategies for Epigastric Hernia
October 19, 2021An epigastric hernia is a condition where a part of the upper abdome...

Understanding Foetal Alcohol Spectrum Disorders: Causes, Effects, and Prevention
August 27, 2021Foetal Alcohol Spectrum Disorders (FASD) encompass a range of lifelo...

Understanding Cleft Lip and Cleft Palate Causes, Symptoms, and Treatment
February 27, 2021As a parent, the wish for a healthy and thriving child is universal....

Premature baby health care at home post-discharge from NICU
May 22, 2019Discharge from the hospital Premature b...

5 Premature Baby Care Tips At Home
February 18, 2019Premature babies are infants that are born about 3 weeks before thei...